Mayo Clinic, the Minnesota-based nonprofit academic health care network with locations in Phoenix and Scottsdale, is expanding its digital health care presence to meet the needs of contemporary consumers and make it easier for rural communities to access necessary care.
The Mayo Clinic Center for Connected Care is developing digital health initiatives, known as telemedicine, to better connect the organization, its providers and its patients.
Under the Center for Connected Care, there are several subcategories: “asynchronous care” does not happen in real-time, meaning a patient can consult a physician or specialist and expect a response within 72 hours; “synchronous care” occurs instantly, so a patient can consult their physician via video conference and get immediate feedback; the Mayo Clinic patient portal and mobile apps allow patients to create an online account through which to track their medical records; and follow-up patient monitoring, which uses a combination of wearable technology (blood pressure cuffs, temperature monitors, etc.) and patient surveys to keep providers updated on the patient’s treatment and recovery.
“Where access to a medical or surgical specialist is an issue, these make even greater sense,” said Dr. Bart Demaerschalk, a Phoenix-based neurologist, professor and medical director of the Mayo Clinic Center for Connected Care. “They obviously don’t fulfill the need for a patient to have a diagnostic test or an intervention or a procedure or a surgery or a more detailed physical examination.”
But, for example, if a patient’s primary care physician or specialist needs a second opinion, an electronic consultation, or e-consult, allows the doctor to reach out and request a second opinion or learn Mayo Clinic best practices for whatever issue they might be addressing, Demaerschalk said.
“It’s an efficient means of receiving expert medical advice without the time and resources and money associated with traveling to a Mayo Clinic site,” he said.
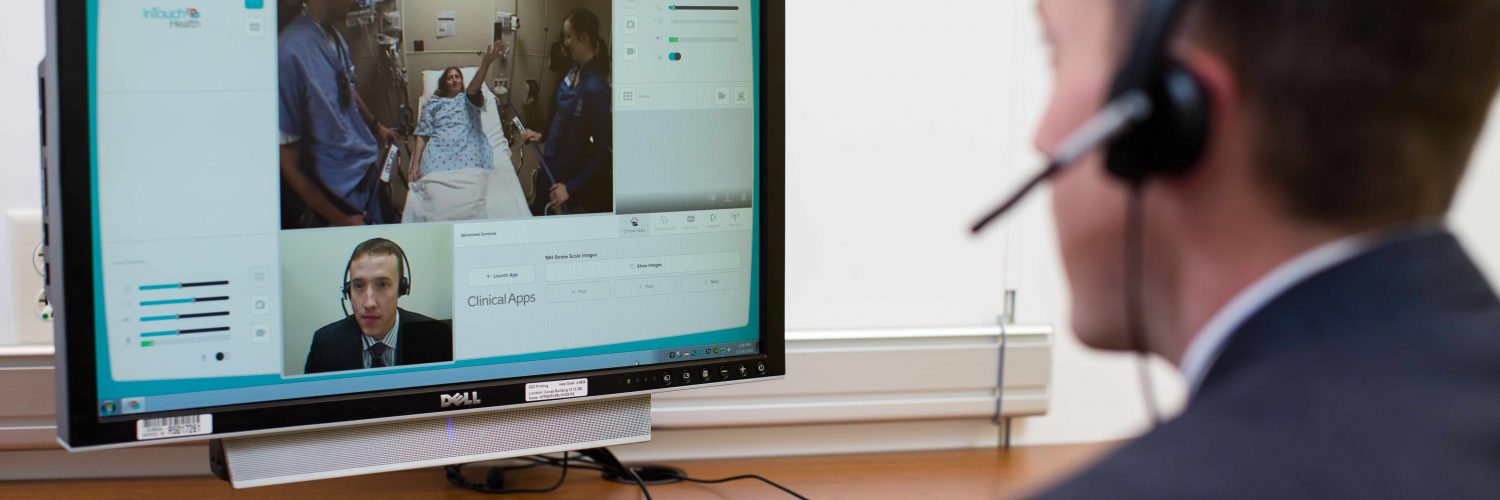
“The same is true for video telemedicine,” he said. “For example, the Mayo Clinic ‘telestroke’ program was born out of the need to provide expert stroke evaluation and management to all the rural patients in Arizona that reside in communities where there are no neurologists or neurosurgeons, where there is not a stroke center.”
Mayo Clinic provides round-the-clock stroke video consultation. Here’s how it works:
“Myself and my colleagues provide a consultation, the physical examination, a review of the brain scans, and we provide in real-time — with a minute response time when an alert is raised to the patient’s emergency physician and nursing staff about the stroke diagnosis — the patient’s eligibility for emergency treatment, and then we help determine whether that patient may need to be transferred to a higher level of care for ongoing treatment or evaluation.”
The telestroke program has been around for 10 years, Demaerschalk said, and it primarily serves rural and remote communities in Arizona as well as parts of Florida and the Midwest. Now, the entire Mayo Clinic health system is employing these strategies to better serve patients and providers alike.
Mayo Clinic is far from alone in its move toward digital health care options.
“There’s definitely been a strong shift toward incorporating digital tools into the practice of medicine,” Demaerschalk said. “Not to replace people or to replace face-to-face interactions, but to complement the health care that currently exists and to overcome some of the obstacles — access being one of them — in remote communities.”
Demaerschalk said he also contributed to legislative changes in Arizona that has made telemedicine more accessible, supporting and assisting the sponsors of two telemedicine bills at the state legislature to ensure that both government and non-government health care insurers reimburse providers “sufficiently, comparably, for a telemedicine consultation, as they would for a face-to-face encounter.”
Mayo Clinic and other health care organizations see other advantages as well, he said.
“For example, there’s recognition today that not all health care delivery necessitates a patient and provider sitting down in a geographic location — in a room, on a campus or in a building — and that good care can be provided at a distance,” Demaerschalk said.
What patients want today is more than just 15 or 30 or 60 minutes sitting in a doctor’s office, he said. They want a dialogue.
“Sometimes, you want your diagnosis to be elaborated upon, you have some questions, you need clarification, some adjustments in your clinical course, and those types of exchanges don’t always necessitate the laying on of hands — a physical examination or a diagnostic test or treatment — and yet, the historical system obligated every patient to travel and then situate themselves, sometimes at their own expense for travel and time,” Demaerschalk said.
Similar to other industries such as finance, travel, real estate and entertainment, consumers are demanding more options, he said. New avenues of communication allow services to be delivered through other means “when it makes sense, wherever it makes sense.”
“It minimizes unnecessary visits, unnecessary clinic appointments,” Demaerschalk said. “It opens up space for other patients that need to occupy a physical clinic or have a physical examination or have a diagnostic test.”
The movement toward digital health care removes the public’s reliance on physical structures — “brick and mortar medicine” — which not only increases access for people who reside far from city centers and large medical facilities but increases individual physicians and specialists’ abilities to reach more patients.
“It’s professionally rewarding and fulfilling to be able to extend my knowledge and expertise and experience to patients that live far away from my geographic clinic practice, and knowing full well that those patients didn’t otherwise have access to a neurologist or a stroke specialist,” Demaerschalk said.
The health care industry’s overall goal in digital medicine is to “improve the health and well-being of our patients,” he said.
Telemedicine is an enhancement or extension of current care options, allowing providers to stay connected with their patients more easily than traditional office visits allow.
“Health care organizations are principally concerned about improving health and well-being and providing access, convenience and lower cost of care by introducing digital health to their traditional health care offerings,” Demaerschalk said.
Photo courtesy of Mayo Clinic















Add comment